Understanding the Trial Results
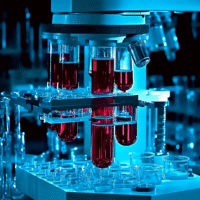
The INHALE WP3 trial looked at a new test called PCR to quickly diagnose hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) in intensive care units (ICUs). Here’s what we learned:
What Worked?
- The PCR test helped doctors use antibiotics more wisely within 24 hours.
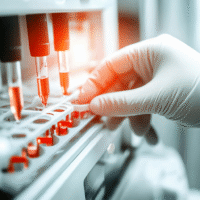
- Using the PCR test resulted in lower overall costs in the ICU, saving about £7,802 per patient compared to standard care.
What Didn’t Work?
- Patients in the PCR group had fewer clinical cures after 14 days compared to those receiving standard treatment.
- While the PCR test was cost-effective for managing antibiotics, it didn’t lead to better recovery rates.
How This Helps Patients and Clinics
This trial shows that while the PCR test can save money and help with antibiotic use, it may not improve the chances of recovery for patients. Clinics can use this information to make better decisions about which tests to use for pneumonia.
Real-World Opportunities
- Hospitals can adopt the PCR test to improve antibiotic management.
- Doctors can use the trial findings to discuss treatment options with patients.
Measurable Outcomes to Track
- Cost savings per patient in the ICU.
- Time taken to start antibiotics after diagnosis.
- Rate of clinical cures at 14 days.
AI Tools to Consider
AI tools can help analyze patient data and predict outcomes, making it easier to decide when to use the PCR test. Look for AI solutions that assist with diagnostic decision-making in pneumonia cases.
Step-by-Step Plan for Clinics
- Start by training staff on the PCR test and its benefits.
- Implement the PCR test in a few selected cases to monitor its effectiveness.
- Collect data on costs, antibiotic use, and patient outcomes.
- Gradually expand the use of the PCR test based on initial findings.
For more detailed information, you can read the full research article here.