Understanding the European Study of Prostate Cancer Screening
What Was the Study About?
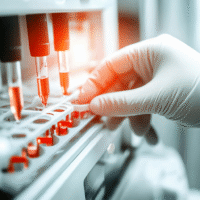
The European Randomized Study of Screening for Prostate Cancer (ERSPC) started in 1993 to see if testing for prostate cancer using a blood test called PSA (prostate-specific antigen) could reduce deaths from this disease. As more people live longer, it’s important to know how effective this testing is.
What Did the Study Find?
After following 162,236 men aged 55 to 69 for 23 years, the study showed:
- Men who were screened had a 13% lower chance of dying from prostate cancer compared to those who were not screened.
- For every 456 men invited for screening, one death from prostate cancer was prevented.
- For every 12 men diagnosed with prostate cancer, one death was averted.
- More men were diagnosed with prostate cancer in the screening group, but this led to fewer deaths.
What Does This Mean for Patients and Clinics?
These results suggest that PSA testing can save lives by reducing prostate cancer deaths. However, it also means that more men will be diagnosed with prostate cancer, which can lead to unnecessary treatments. Clinics should focus on balancing the benefits of screening with the risks of overdiagnosis.
Real-World Opportunities
- Hospitals can implement regular PSA screening for men aged 55 to 69.
- Doctors can educate patients about the benefits and risks of PSA testing.
- Clinics can develop personalized screening plans based on individual risk factors.
Measurable Outcomes to Track
- Number of men screened for prostate cancer.
- Number of prostate cancer diagnoses made.
- Reduction in prostate cancer mortality rates.
- Patient satisfaction with screening and follow-up care.
AI Tools for Implementation
Consider using AI tools to analyze patient data and identify those at higher risk for prostate cancer. These tools can help in creating personalized screening schedules.
Step-by-Step Plan for Clinics
- Start by educating your staff about the benefits of PSA screening.
- Begin a pilot screening program for men aged 55 to 69.
- Monitor outcomes and gather feedback from patients.
- Adjust the program based on results and patient needs.
- Gradually expand the program to include more patients and risk assessments.
Learn More About the Research
For more details, you can read the full study here.